Roger D. Kamm, Ph.D.
AIMBE College of Fellows Class of 1993 For contribution to fundamental understanding of the ventilation of the lung.
Roger Kamm elected to the National Academy of Engineering for 2023
Via MIT | February 14, 2023Seven MIT researchers are among the 106 new members and 18 international members elected to the National Academy of Engineering (NAE) this week. Fourteen additional MIT alumni, including one member of the MIT Corporation, were also elected as new members.
One of the highest professional distinctions for engineers, membership to the NAE is given to individuals who have made outstanding contributions to “engineering research, practice, or education, including, where appropriate, significant contributions to the engineering literature” and to “the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education.” The seven MIT researchers elected this year include:
……
Roger D. Kamm SM ’73, PhD ’77, the Cecil and Ida Green Distinguished Professor of Biological and Mechanical Engineering, for contributions to the understanding of mechanics in biology and medicine, and leadership in biomechanics… Continue reading.
Engineers develop nanoparticles that cross the blood-brain barrier
Via MIT | June 1, 2022There are currently few good treatment options for glioblastoma, an aggressive type of brain cancer with a high fatality rate. One reason that the disease is so difficult to treat is that most chemotherapy drugs can’t penetrate the blood vessels that surround the brain.
A team of MIT researchers is now developing drug-carrying nanoparticles that appear to get into the brain more efficiently than drugs given on their own. Using a human tissue model they designed, which accurately replicates the blood-brain barrier, the researchers showed that the particles could get into tumors and kill glioblastoma cells… Continue reading.
Cancer cells soften as they metastasize, study suggests
Via MIT | April 20, 2021When cancer cells metastasize, they often travel in the bloodstream to a remote tissue or organ, where they then escape by squeezing through the blood vessel wall and entering the site of metastasis. A study from MIT now shows that tumor cells become much softer as they undergo this process.
The findings suggest that drugs that prevent cells from softening could potentially slow or halt metastasis. Metastatic tumors are estimated to be present in about 90 percent of patients who die of cancer.
“We have long thought that if we could identify the barriers that a cancer cell has to overcome to form a metastatic tumor, that new drugs could be found and lives could be saved,” says Roger Kamm, the Cecil and Ida Green Distinguished Professor of Biological and Mechanical Engineering and an author of the study… Continue reading.
Tissue model reveals role of blood-brain barrier in Alzheimer’s
Via MIT | August 12, 2019Beta-amyloid plaques, the protein aggregates that form in the brains of Alzheimer’s patients, disrupt many brain functions and can kill neurons. They can also damage the blood-brain barrier — the normally tight border that prevents harmful molecules in the bloodstream from entering the brain.
MIT engineers have now developed a tissue model that mimics beta-amyloid’s effects on the blood-brain barrier, and used it to show that this damage can lead molecules such as thrombin, a clotting factor normally found in the bloodstream, to enter the brain and cause additional damage to Alzheimer’s neurons… Continue reading.
Understanding and treating disease
Via MIT | February 2, 2018……
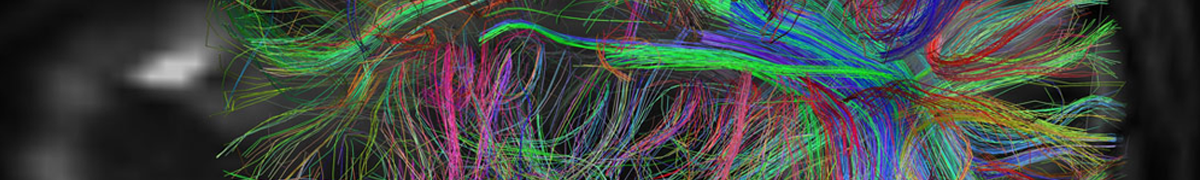
While improving diagnostic methods could help catch a disease early, tracking how diseases grow could be key to developing new therapeutic interventions. Roger Kamm, the Cecil and Ida Green Distinguished Professor, and his lab use a device that’s roughly the size of a quarter to track tumor cells as they leave the vascular network and eventually grow into tumors. These tiny microfluidic devices can help us understand how cancer metastasizes.
“We’ve developed a 3-D vascularized network in which we can track cancer cells inside a capillary,” says Kamm. “It’s about understanding how cell populations interact. We can watch the tumor cells escape from the vessel to invade the surrounding tissue.”
The microfluidic device consists of two media channels on either side with 3-D hydrogel in the center. The gel is seeded with endothelial cells that form capillaries where the tumor cells are introduced. From there, Kamm and his team use microscopic imaging to watch every single movement the tumor cell makes. From intravasation — when a cancer cell enters the bloodstream — to extravasation — when a tumor cell leaves the blood stream and becomes metastatic — the cell’s path is studied with painstaking precision… Continue reading.
A Microchip for Metastasis: MIT researchers design a microfluidic platform to see how cancer cells invade specific organs
Via Massachusetts Institute of Technology | February 2, 2014Nearly 70 percent of patients with advanced breast cancer experience skeletal metastasis, in which cancer cells migrate from a primary tumor into bone — a painful development that can cause fractures and spinal compression. While scientists are attempting to better understand metastasis in general, not much is known about how and why certain cancers spread to specific organs, such as bone, liver, and lungs.
Now researchers from MIT, Italy, and South Korea have developed a three-dimensional microfluidic platform that mimics the spread of breast cancer cells into a bonelike environment.
The microchip — slightly larger than a dime — contains several channels in which the researchers grew endothelial cells and bone cells to mimic a blood vessel and bone side-by-side. They then injected a highly metastatic line of breast cancer cells into the fabricated blood vessel.
Twenty-four hours later, the team observed that twice as many cancer cells had made their way through the vessel wall and into the bonelike environment than had migrated into a simple collagen-gel matrix. Moreover, the cells that made it through the vessel lining and into the bonelike setting formed microclusters of up to 60 cancer cells by the experiment’s fifth day.
“You can see how rapidly they are growing,” says Jessie Jeon, a graduate student in mechanical engineering. “We only waited until day five, but if we had gone longer, [the size of the clusters] would have been overwhelming.”
The team also identified two molecules that appear to encourage cancer cells to metastasize: CXCL5, a protein ligand secreted by bone cells, and CXCR2, a receptor protein on cancer cells that binds to the ligand. The preliminary results suggest that these molecules may be potential targets to reduce the spread of cancer.
Jeon says the experiments demonstrate that the microchip may be used in the future to test drugs that might stem metastasis, and also as a platform for studying cancer’s spread to other organs.
She and her colleagues, including Roger Kamm, the Cecil and Ida Green Distinguished Professor of Mechanical and Biological Engineering at MIT, have outlined the results of their experiments in the journal Biomaterials.
 AIMBE
AIMBE
