Warren M. Grill, Ph.D.
AIMBE College of Fellows Class of 2007 For fundamental contributions to the development of novel technologies for functional electrical stimulation to restore organ function.
Light-based DBS Method Can Alleviate Motor Symptoms of Parkinson’s, Animal Study Shows
Via Parkinsons News Today | May 5, 2020Scientists have developed a new light-based deep brain stimulation method that when applied to neurons located in the subthalamic nucleus (STN) — a brain region involved in controlling movement — alleviated motor symptoms in a rat model of Parkinson’s disease.
The study detailing that research, “Frequency-Specific Optogenetic Deep Brain Stimulation of Subthalamic Nucleus Improves Parkinsonian Motor Behaviors,” was published in The Journal of Neuroscience.
Deep brain stimulation (DBS) is a surgical treatment for Parkinson’s disease that involves implanting a device to activate specific regions of the brain with electrical signals generated by a battery-operated neurostimulator… Continue reading.
Understanding Deep Brain Stimulation
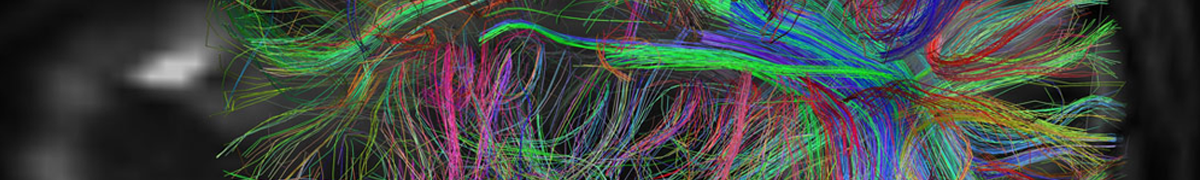
Via Duke News | June 23, 2015For the past 17 years, neurosurgeons have implanted electrodes into the brains of persons with Parkinson’s disease to deliver a constant barrage of electric impulses. For many patients, the treatment known as Deep Brain Stimulation (DBS) immediately relieves the motor impairment caused by the disease.
Warren Grill, professor of biomedical engineering and neurobiology at Duke University and member of the Duke Institute for Brain Sciences, is working to understand the mechanisms of DB) and use this understanding to develop innovative improvements to the therapy.. And thanks to a prestigious new $4 million grant called the Javits Neuroscience Investigator Award, Grill will delve further into the mystery than ever before.
The Javits Award is a four-year grant that can be extended to seven years that is given by the National Institute of Neurological Disorders and Stroke (NINDS), which is an arm of the National Institutes of Health (NIH). The award is given to scientists for their “superior competence and outstanding productivity,” and it “provides long-term support to investigators with a history of exceptional talent, imagination, and preeminent scientific achievement.”
“The goal of our research is to do a better job at relieving the symptoms of Parkinson’s disease and essential tremor and to do so with less energy,” said Grill. “This will allow us to improve patient outcomes and to make smaller and longer lasting battery-powered implants.”
Previous research has shown that DBS is effective only at frequencies of more than 100 pulses per second, which quickly depletes the battery of the implanted stimulator. Grill’s work, however, has demonstrated that lower frequencies can be effective if an appropriately designed temporal pattern is used—analogous to a Morse code of electric pulses.
Fixing the Signal
Via Proto | April 16, 2015IN ANOTHER EFFORT TO FIND and explore specific neural neighborhoods, Warren Grill, a professor of biomedical engineering at Duke University, is working on electrical stimulation to treat urinary incontinence. That starts with understanding the changes in neural signaling that take place during bladder filling and emptying, both in healthy and overactive bladders.
Grill records those signals, primarily in rats, using two basic methods to get a range of perspectives. The first is to place a cuff electrode around pelvic, hypogastric or pudendal nerves, all thought to be involved in bladder regulation. That electrode captures all of the activity in the nerve. “It’s like listening to the entire orchestra at once,” Grill says. To complement that aggregate signal, Grill also uses novel probes developed by Tim Gardner, an assistant professor of biology at Boston University, which let him record activity from single nerve fibers. “That’s like listening to just the first piccolo or the third trumpet,” Grill says. “We can record up to 16 channels simultaneously.” Ultimately, he hopes to translate this research into a closed-loop device that provides more effective, dynamic relief for patients than they get from current open-loop systems. (Closed-loop systems can both read and send electrical signals automatically.)
On Top of Neuro-Engineering, in the Lab and the Classroom
Via Duke | September 18, 2014Warren Grill isn’t a great tennis player, and he knows why. It’s all about practice.
“Watching the U.S. Open on television, the sport looks pretty easy,” said Grill, a professor of biomedical engineering and a Bass Fellow. “But when you get out on the court, hitting the ball is hard. The only way to get better is practice. Unfortunately, when it comes to tennis, I need to practice a lot more.”
Grill translates that theory in his classroom, where his Duke students get plenty of engineering practice. He teaches an undergraduate core biomedical engineering course on bioelectricity and a graduate level course on neural prosthetics, his area of expertise. In both, he tries to keep the lectures to a minimum and emphasizes problem-solving.
“Making mistakes is valuable in engineering education,” said Grill, who often challenges his upper-level students with unsolved problems from current research. “Engineering is all about problem-solving. Too often, students are afraid to fail, and it leads to a fear of initiating new approaches. But what they need to see is even the best engineers have to make multiple failed attempts at a problem before arriving at a successful approach.
 AIMBE
AIMBE
